What Happens During Reconstructive Surgery
What happens during reconstructive surgery after breast cancer depends on the type of surgery you have. You can opt for reconstructive surgery using artificial implants. Or you can choose to have surgery that rebuilds your breast mound or shape using tissue from another part of your body. Here are descriptions of the more common types of surgery used today.
What happens when you get implants
If your skin and chest wall tissues are tight and flat, you may need a tissue expander, which is kind of like a balloon. First, you are put to sleep using drugs called general anesthesia. Then, the surgeon implants the expander beneath your skin and chest muscle. Over a period of weeks or months, a surgeon injects salt water called saline into the tissue expander. This is often performed during an office visit.
These injections stretch your skin and muscle to the size needed for the new breast mound. Once the skin has stretched enough, you may have a second surgery. During this surgery, the surgeon removes the tissue expander and inserts the permanent implant beneath your muscle and skin. The implant is usually a silicone sac filled with saline solution or silicone gel. You'll go home the same day that the surgery is done. In some cases, the tissue expander serves as the final implant.
Implant with latissimus dorsi reconstruction
The latissimus dorsi is a large, fan-shaped muscle on your back, below your shoulder. Your surgeon may do this kind of reconstruction when it's not possible to use your existing chest muscle or skin to cover an implant. Your surgeon uses this muscle to create a new breast mound. Because the latissimus is not large enough to make a breast shape in most women, the surgeon also places an implant under the muscle. If you have this type of surgery, you'll have a scar on your back as well as on your chest.
What happens when you get tissue flap breast reconstruction
Instead of having artificial implants inserted, you can have a new breast mound built or constructed using your own tissue. The tissue may come from your abdomen (belly) or buttocks.
-
Transverse rectus abdominus muscle (TRAM) flap. The surgery also gives you a tummy tuck. During this procedure, one of two muscles from your abdomen, along with skin and fat, is transferred to your mastectomy site. 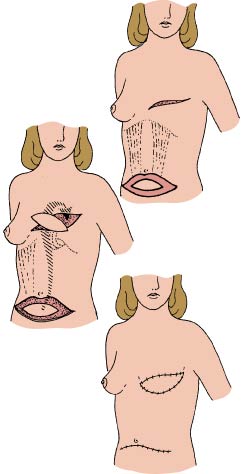 When this tissue is cut free from its original location, it's called a free flap. Or the tissue can be tunneled under the skin to the breast area. Your surgeon shapes this muscle, skin, and fat into a breast shape, so you may not need an implant. Transferring this tissue also causes a tightening of your stomach. TRAM flaps tend to behave more like the rest of your body tissue, for example, they may change as you gain and lose weight. The procedure itself is more complicated and requires more time in the operating room. This may not be a good choice for women who have back problems because removing stomach muscles can increase stress on the back. If you have this type of surgery, you'll have a horizontal scar across your lower abdomen plus a scar on your chest.
When this tissue is cut free from its original location, it's called a free flap. Or the tissue can be tunneled under the skin to the breast area. Your surgeon shapes this muscle, skin, and fat into a breast shape, so you may not need an implant. Transferring this tissue also causes a tightening of your stomach. TRAM flaps tend to behave more like the rest of your body tissue, for example, they may change as you gain and lose weight. The procedure itself is more complicated and requires more time in the operating room. This may not be a good choice for women who have back problems because removing stomach muscles can increase stress on the back. If you have this type of surgery, you'll have a horizontal scar across your lower abdomen plus a scar on your chest.
-
Gluteal free flap. The free flap is a newer technique in reconstructive surgery. The surgeon removes part of the skin and fat from your buttocks, and grafts it onto the mastectomy site. This is a more complex operation, sometimes requiring two teams of surgeons. One team may remove the flap, and the second prepares the blood vessels. As with a TRAM free flap, its success depends on tissues getting proper nourishment from the blood vessels.
-
Deep inferior epigastric perforator (DIEP) flap. For this newer procedure, the surgeon detaches blood vessels and surrounding fat and skin in your lower abdomen and moves them to the mastectomy site. Abdominal muscle is left intact, but blood vessels must first be dissected from the muscle.
In addition to these reconstructive surgical operations, you may decide to have other procedures to improve how your new breast looks. For example, you might decide to have reconstructive surgery on your other breast so that it matches your new breast. Or you may want to have a nipple reconstructed.
Schedule a Mammogram at Richmond University Medical Center
Early detection and treatment is the best strategy for a better cancer outcome. Schedule your mammogram at RUMC: Call 718-818-3280.
Kathy Giovinazzo is Director of Radiology at Richmond University Medical Center.
For More Information
For more information or to schedule an appointment, contact Dr. Thomas Forlenza at 718-816-4949. His office is located at 1366 Victory Blvd on Staten Island.
Dr. Forlenza is the Director of Oncology at Richmond University Medical Center.